Understanding Hand, Foot, and Mouth Disease (HFMD)
Hand, foot, and mouth disease (HFMD) is a common viral infection in children. HFMD is common in babies and children younger than 5 years old, but older children can get it. Occasionally adults will get it.
HFMD can cause mouth sores and a painless rash on the hands, feet, or buttocks. It can be easily spread from one person to another. HFMD is often mistaken for strep throat because the symptoms of both conditions are similar. HFMD can cause some discomfort, but it’s not a serious problem. Most cases can easily be managed and treated at home.
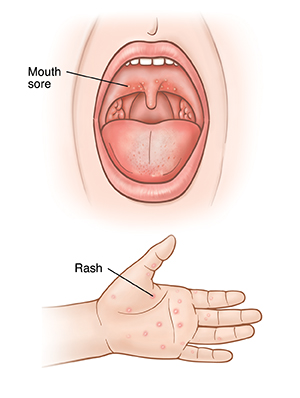 |
| HFMD can cause mouth sores and a rash on areas such as the hands, feet, or buttocks. |
What causes HFMD?
HFMD is most often caused by the coxsackievirus A16. It can also be caused by other viruses in the same family as coxsackievirus. HFMD is spread in one of these ways:
-
Breathing infected air. The virus can enter the air when an infected person coughs, sneezes, or talks.
-
Contact with contaminated items. Some things may have traces of stool from an infected person. This can occur when an infected person doesn’t wash their hands after having a bowel movement or changing a diaper.
-
Contact with fluid from the blisters. The blisters are part of the rash. This type of transmission is rare.
What are the symptoms of hand, foot, and mouth disease?
Symptoms usually appear 24 to 72 hours after contact. They include:
-
Rash of small, red bumps or blisters on the hands, feet, or buttocks
-
Mouth sores that often occur on the gums, tongue, inside the cheeks, and in the back of the throat (mouth sores may not occur in some children)
-
Sore throat
-
A rash over the rest of the body
-
Fever
-
Loss of appetite
-
Pain when swallowing
-
Drooling
How is HFMD diagnosed?
HFMD is diagnosed by how the rash and mouth sores look. The healthcare provider will ask about you or your child’s symptoms and health history. They will also examine you or your child. You will be told if any tests are needed. These are done to rule out other infections.
How is HFMD treated?
There is no specific treatment for HFMD. But there are things you can do at home to help relieve some symptoms. The illness lasts about 7 to 10 days. Your child is no longer contagious 24 hours after the fever is gone. You can take steps to relieve symptoms and prevent dehydration while you or your child are sick.
Mouth pain
-
Use ibuprofen or acetaminophen to treat pain or discomfort. Or use the medicine prescribed by the healthcare provider for pain. Talk with your child's provider about the dose and when to give the medicine (schedule). Do not give ibuprofen to a baby age 6 months or younger. Don't give aspirin to a child 19 years or younger with a fever. This can put them at risk for a serious illness called Reye syndrome. This condition affects the liver and brain.
-
Liquid antacid can be used 4 times per day. This is used to coat the mouth sores for pain relief. Talk with your child's provider about how much and when to give the medicine to your child:
-
Children older than age 4 can use 1 teaspoon (5 mL) as a mouth rinse after meals.
-
For children younger than age 4, a parent can place ½ teaspoon (2.5 mL) in the front of the mouth after meals. Don't use regular mouth rinses. They may sting.
Stay hydrated
-
Follow a soft diet with plenty of fluids to prevent too much fluid loss (dehydration). If you or your child doesn't want to eat solid foods, it's OK for a few days, as long as they drink plenty of fluids.
-
Drink cool fluids and eat frozen treats such as sherbet. These are soothing and easier to take.
-
Avoid citrus juices such as orange juice or lemonade and salty or spicy foods. These may cause more pain in the mouth sores.
When to get medical care
Call your healthcare provider if you or your child has any of these:
-
A mouth sore that doesn’t go away within 14 days
-
Increased mouth pain
-
Trouble swallowing
-
Neck pain
-
Chest pain
-
Trouble breathing
-
Weakness
-
Lack of energy
-
Signs of infection around the rash or mouth sores, such as pus, fluid leaking, or swelling
-
Signs of too much fluid loss, such as very dark or little urine, excessive thirst, dry mouth, dizziness
-
A fever that lasts longer than 3 days (see Fever and children below)
-
A seizure
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider
How can HFMD be prevented?
HFMD is very contagious. If you or your child have HFMD, follow these steps to keep from passing it to others:
-
Wash your hands well with soap and clean, running water. Teach your child to wash their hands with soap and clean, running water often. Wash your hands for at least 20 seconds. Handwashing is very important before eating or handling food, after using the bathroom, and after touching the rash. A child is very contagious during the first week of the illness. They can still be contagious for days to weeks after the illness goes away.
-
Clean and disinfect frequently touched surfaces and shared items, such as toys and doorknobs.
-
Don't share cups, utensils, or napkins. Don't share personal items such as towels and toothbrushes.
-
Ask your child's healthcare provider how long your child should avoid school, daycare, and playing with others. Because HFMD is normally mild, most kids can go to daycare or school as long as they have no fever, no uncontrolled drooling from mouth sores, and feel well enough to join activities. But always check with your daycare or school for their guidelines.
If you are well but around others with HFMD, avoid touching your nose, eyes, and mouth with unwashed hands. Do not hug or kiss someone who has HFMD and don't share personal items.