When Your Child Has Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea (OSA) is a fairly common problem in children. But it often goes undiagnosed. This is partly because symptoms can be different than they are in adults. OSA occurs when the airway becomes blocked during sleep. When this happens, the brain tells the body to wake up just enough to open the airway and allow breathing again. This can happen many times during the night, even if your child doesn’t remember it. The quality of sleep can be very poor.
What causes OSA in children?
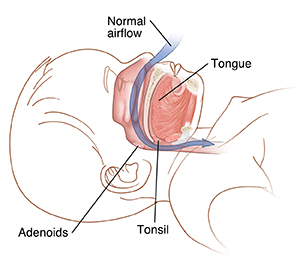
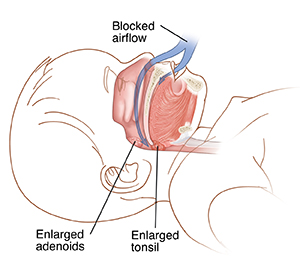
In children, enlarged tonsils and adenoids are the most common cause of sleep apnea. These are normal gland structures in the back of the throat. When muscle tone is relaxed during sleep, throat tissues may collapse on the enlarged glands and can cause a full or part blockage of airflow. Being overweight can also make sleep apnea more likely. But extra weight is a less common cause of OSA in children than it is in adults. In some children, the shape of the face, jaw, or tongue leads to a blocked airway during sleep. Your child’s healthcare provider can tell you more about what’s causing your child’s sleep apnea.
What are the symptoms of OSA?
-
Snoring, gasping, or snorting, along with periods of not breathing
-
Breathing through the mouth, at night and during the day
-
Restless sleep, or sleeping in unusual positions
-
Nighttime sweating
-
Bedwetting
-
Trouble waking up in the morning
-
Daytime sleepiness or irritability
-
Headaches in the morning
-
Hyperactivity and trouble paying attention
-
Learning problems
How is OSA diagnosed?
The healthcare provider may refer your child to a healthcare provider with special training in sleep disorders. Or your child may see an ear, nose, and throat provider (otolaryngologist). To diagnose sleep apnea, the healthcare provider asks about your child’s health history and sleep habits. They examine and weigh your child. Your child may have an overnight sleep study (polysomnography).
What is an overnight sleep study?
To confirm a diagnosis, your child will need an overnight sleep study. This is done in a sleep lab, which may be located in a hospital or special clinic. Bring pajamas for your child, as well as something that will help your child feel more comfortable, such as a stuffed animal. You will be able to sleep in a bed near your child. You can help prepare your child by describing in advance and in an age-appropriate manner as much as you can: Tell your child who will be present and where you will be. Answer your child’s questions and use pictures to help explain the procedure, if that’s helpful. During the sleep study, electrodes and sensors are attached to your child’s body. They measure many things, including:
-
Activity of your child’s brain and muscles
-
Electrical activity of your child’s heart
-
Oxygen content in your child’s blood
-
Movement of the chest and abdomen
-
Airflow through the mouth and nose
-
Number of part or full airway blockages during the night
How is OSA treated?
Treatment depends on your child’s age, health, and medical history, as well as any underlying conditions. Your child’s healthcare provider may suggest the following:
-
Surgery to remove tonsils (tonsillectomy) and adenoids (adenoidectomy)
-
Continuous positive airway pressure (CPAP), a machine that sends pressurized air through a facemask as you sleep
-
Losing excess weight
What are the long-term concerns?
Left untreated, OSA can cause growth, learning, and behavior problems. It can even cause heart problems. But treatment can help prevent these problems, make them less severe, or make them go away. Follow treatment advice, keep follow-up appointments, and call the healthcare provider if your child has new symptoms. Also call the healthcare provider if you have any questions.